Diseases
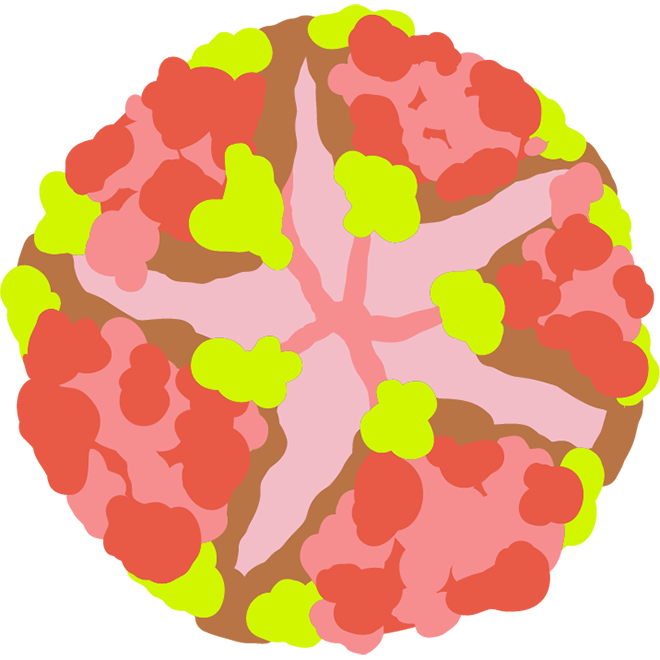
Viruses, pathogens
Our society is facing new ecological challenges due to the changing climate and increasing global trade. Over the last decade, the distribution, annual reproduction cycle and density of many arthropod species important for the spread of human, animal or plant pathogens have changed. Therefore, the risk of emerging infectious diseases is increasing in temperate regions, including Europe and Hungary. The greatest threat in our country is related to the ecological processes in biting midge and tick populations, but many other arthropods and other vector species may also be affected. This applies not only to native species – we must also take into account the risks posed by newly established invasive species, which include the spread of more serious tropical diseases hitherto unknown in our country.
CHIKUNGUNYA FEVER
DISTRIBUTION
In Europe, it first appeared in 2007 in the Italian region Emilia-Romagna and then in France. Outbreaks of Chikungunya similar to those in Italy and France are expected in our country as well.
AFFECTED HOST SPECIES
The main host of the virus, which causes about three million infections each year, are humans, but in Africa non-human primates can also serve as primary hosts. In other cases, the chikungunya virus can also be found in birds and other vertebrates.
TRANSMISSION AND VECTORS
It is spread by mosquitoes of the genus Aedes. The main vector species responsible for outbreaks are the yellow fever mosquitoes (Aedes aegypti) and the Asian tiger mosquitoes (Aedes albopictus). Mother-to-newborn transmission is rare, but the virus can be passed during breastfeeding.
SYMPTOMS
Approximately 3–28% of people infected with chikungunya virus remain asymptomatic. The incubation period for people with the disease is usually 3-7 days. This may be followed by symptoms such as high fever, chills, headache, conjunctivitis, excessive sensitivity to light and arthritis. The fever usually subsides after 2–3 days. 80% of patients may suffer from persistent joint pain and prolonged fatigue, which can last for years. Children and the elderly are at higher risk, with a longer recovery period. There is a risk of developing severe disability, chronic joint pain and complications as a result of the infection.
TREATMENT, PREVENTION
There is one vaccine (Ixchiq), approved by the FDA in 2023, available to persons over the age of 18, a single dose is sufficient for long-term immunity, contains a weakened virus, and medication can be used to relieve symptoms. During the first week of infection, patients carry high levels of the virus in their blood, so mosquito bites should be avoided to prevent further transmission. Prevention is the most effective method of protection.
DENGUE FEVER
DISTRIBUTION
Dengue fever occurs frequently in more than 110 countries, mostly in Asia, in the Pacific and Caribbean regions, America, and Africa. It is highly mobile, spreading by infected travellers as well. The number of infectious cases has increased dramatically over the last few decades, and large epidemics have occurred. It can be brought into the EU by infected tourists returning home but locally acquired cases are also increasing. In 2024, Europe recorded 213 cases in Italy, 85 in France, and 10 in Spain. The risk of transmission by blood donation is currently under investigation.
AFFECTED HOST SPECIES
Its main hosts are humans. In tropical and subtropical areas, it spreads and survives in a human-mosquito cycle. Cases indicating illness in non-human primates have been found in Southeast Asia and West Africa, but there is no evidence that they are responsible for the development of major epidemics.
TRANSMISSION AND VECTORS
Humans can be infected by bites from the Asian tiger mosquito (Aedes albopictus) or the yellow fever mosquito (Aedes aegypti). Dengue fever is only transmitted by the bite of an infected virus-carrying mosquito. The risk is higher in populated areas because the yellow fever mosquito species is found in urban environments.
SYMPTOMS
In 40-80% of cases, the infection is asymptomatic. After a latency period of eight to ten days, mild and usually flu-like symptoms may appear. Clinical symptoms include sudden fever, severe headache, eye socket pain, muscle pain, joint pain, skin rashes, and mild bleeding. Dengue fever is also known as “break-bone fever” because it can cause such severe pain that the patient feels as if his bones are breaking. The illness rarely lasts longer than ten days, but recovery can take a long time. Usually less than 5% of cases cause serious illness, and a fraction of these result in death, mainly among children and adolescents. A more serious form of dengue fever is dengue hemorrhagic fever or dengue shock syndrome (DHF/DFF), which is associated with increased vascular permeability and thus life-threatening bleeding.
TREATMENT, PREVENTION
Currently, two vaccines are available, one is Dengvaxia, which can be given to children aged 9–16 only if they have already had a dengue infection and live in a high-risk area, the other is Qdenga, which can be given from the age of 4, and contains a weakened virus. An important element of prevention is protection against mosquito bites. Infection can be detected serologically by identifying specific antibodies about 5–6 days after infection.
DIROFILARIOSIS
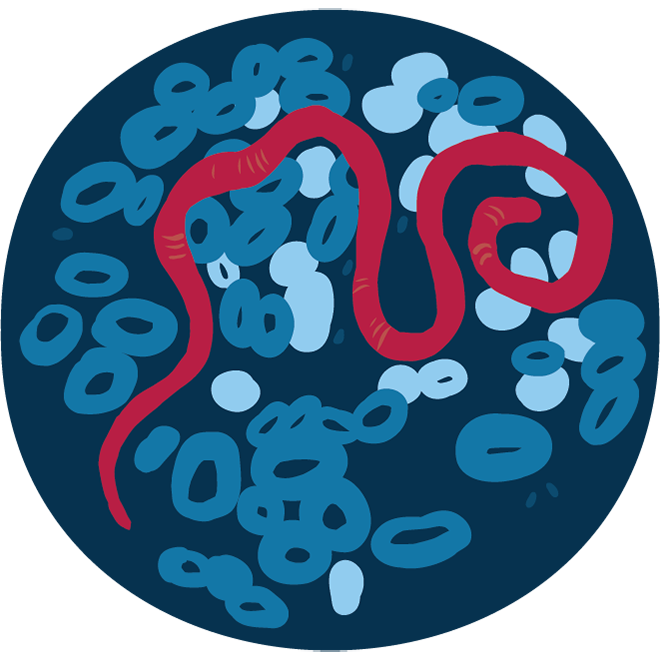
DISTRIBUTION
Heartworm disease and subcutaneous dirofilariasis are common in subtropical countries; however, they are appearing more and more frequently in Europe as well. It is mainly common in the southern part of the continent, but more and more reports are coming from countries further north. In our country, subcutaneous dirofilariasis caused by Dirofilaria repens has been known for decades. The first observation of Dirofilaria immitis in Hungary occurred in the last decade. Climate change plays a role in the increasing number of cases caused by these two Dirofilaria species.
AFFECTED HOST SPECIES
Mosquito vectors are essential to the developmental cycle of Dirofilaria species, which can infect dogs, wild carnivores, and rarely humans. Many other mammalian species are susceptible to infection, such as cats, bears, golden jackals, weasels, ferrets and rodents. Carnivores, especially dogs, can become infected with subcutaneous dirofilariasis without showing any symptoms, and rarely humans can be affected, too, with less severe symptoms. Based on national data, 563 dogs were found to have subcutaneous dirofilariasis between 2006 and 2009. Heartworm disease in dogs infected in this country was first detected in 2007. Since then, an increasing number of dogs have been diagnosed with heartworm disease caused by Dirofilaria immitis.
Transmission AND VECTORS
The infection is transmitted by mosquitoes, with nearly seventy mosquito species potentially capable of spreading it. In Hungary, Dirofilaria species have been confirmed in several species, mostly in Aedes spp., and Culex species.
SYMPTOMS
In humans, symptoms appear after 2-3 months following infection with Dirofilaria immitis. The larvae can cause lesions by reaching the lungs. Symptoms may include cough and chest pain, fever. In dogs, it can be asymptomatic for years; however, most cases are characterised by allergic reactions, fever, high blood pressure, inadequate blood supply to the right side of the heart, anaemia, dead worms can cause embolism or even sepsis, heart failure, inflammation of the liver and kidneys caused by vascular blockage. In cats, the disease mainly affects the lungs. In humans, the presence of Dirofilaria repens is often completely asymptomatic; if it does occur, the parasite causes local swelling and subcutaneous nodules. Chronic cough, shortness of breath, fatigue, weakness, loss of appetite, weight loss, fever, suppuration of the infected area, eczema, oedema may occur. In our country, 118 human cases caused by Dirofilaria repens were reported between 2001 and 2018, most of them involving subcutaneous connective tissue, eyes and less frequently lymph nodes and lungs. In pets (dogs and cats), allergies, itching and hair loss occur in the affected area.
TREATMENT, PREVENTION
The emphasis should be on prevention. Medicinal treatments can help to kill the worms, but may pose serious risks, as dead and drifting worms can cause pulmonary embolisms and instant death in dogs. In some cases, adult worms are removed surgically. There is no vaccination.
MALARIA
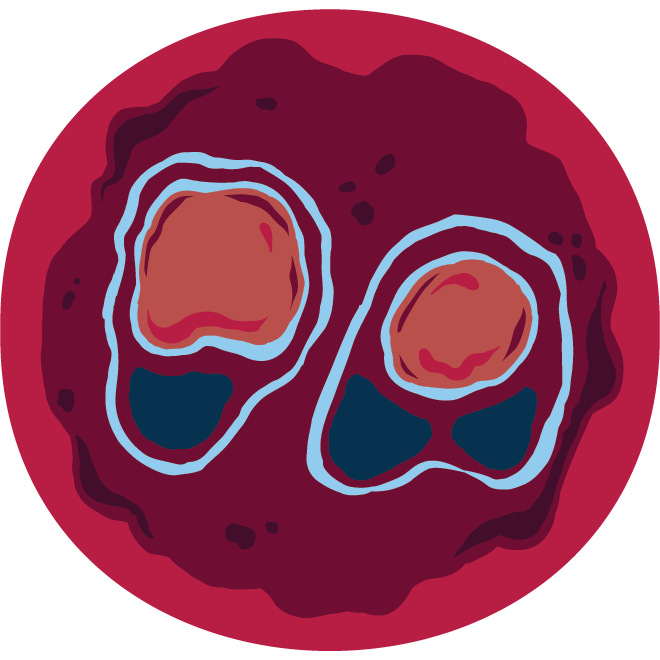
DISTRIBUTION
The pathogen is native to Central and South America, Africa and Asia. The disease was eradicated in Europe by the 1970s, but in recent years there has been an increase in the number of imported cases. The latter poses an increasing threat, because spread by local mosquitoes, secondary infections develop from imported cases, as a result of which a fatal case has already been recorded. Malaria was also present in Hungary for centuries. The last case was in 1959, and the WHO declared the country malaria-free in 1963. Currently, the number of imported cases is low.
AFFECTED HOST SPECIES
Four Plasmodium species, including P. falciparum, P. vivax, P. ovale, and P. malariae only infect humans. However, several other Plasmodium species are specialized to infect different vertebrate groups, such as monkeys, rodents, and birds, and have similar life cycles. These species do not pose a risk to humans.
TRANSMISSION AND VECTORS
Its most common vectors are the Anopheles mosquitoes, which are also native to Hungary (several species are known, most of which do not feed on human blood), but it can also be transmitted through blood transfusions or during childbirth.
SYMPTOMS
The main symptom of malaria is fever, usually a typical fever attack accompanied by chills. In addition, muscle pain, headache, malaise, sweating, fatigue, dizziness, muscle and joint pain, possibly dry cough and gastrointestinal complaints, loss of appetite, nausea, vomiting, and abdominal cramps may occur. Complications of infection with P. falciparum species can even result in death.
TREATMENT, PREVENTION
The disease can be cured with timely medication. Two vaccines have been developed: the RTS,S/Mosquirix, which is given to children, 3 doses are required before the age of 2, then a fourth one will provide additional protection for another 1-2 years, reduces the risk of serious illness requiring hospitalisation by 30%; the other, R21/Matrix-M, which has a higher efficiency of 77% according to tests. efficiency. In addition, protection against mosquitoes that spread malaria also plays an important role in prevention.
USUTU
Distribution
In Europe, it was first detected in Austria in 2001. However, a retrospective analysis revealed it in a bird tissue sample collected in 1996 from the Tuscany region of Italy. In Hungary, Usutu virus was first identified in a blackbird in 2005; this deceased bird was found in Budapest’s 11th district. In 2006, Usutu virus–infected blackbird carcasses were also found in Budapest’s 16th and 18th districts.
Affected Host Species
The virus primarily infects birds but can also cause symptoms in mammals and humans. In Europe, it has been detected in 28 wild bird species to date. Taxonomically and ecologically, the virus closely resembles West Nile virus. However, unlike West Nile virus, Usutu virus rarely causes disease in humans, and then primarily in individuals with weakened immune systems. In Hungary, the virus was first detected in human blood in 2018. However, similarly to West Nile virus, all non-avian hosts are considered dead-end hosts, meaning they cannot transmit the virus to others.
Transmission and Vectors
Its vectors are mainly mosquitoes, similar to West Nile virus. Usutu virus has been isolated from numerous mosquito species, with the common house mosquito (Culex pipiens) likely being the most common vector.
Symptoms
Usutu virus infections produce symptoms similar to those of West Nile virus. In birds, the infection manifests as neurological signs, as well as enlargement and inflammation of internal organs (liver, spleen, heart). In humans, most infections are asymptomatic. Some patients may experience general malaise, headache, fever, muscle pain, and occasionally rashes. The disease typically resolves on its own within 1–2 weeks.
Treatment and Prevention
There is no vaccine against Usutu virus. In most cases, the disease resolves spontaneously. There are no reports in the literature of severe complications requiring medical treatment.
WEST NILE FEVER
Distribution
In Europe, the virus was first detected in a human patient in Albania in 1985. Today, however, these are one of the most widespread flaviviruses in Africa, the Middle East, and Europe. In Hungary, it was first identified in rodents in the 1970s, but it did not cause clinical disease in the country until 2003. Data on human cases in Hungary have been available since 2003, and since 2012, West Nile virus infections have been classified as notifiable diseases. Until 2017, the number of reported cases per year was well below fifty, but in 2018, there were already 225 cases, fifteen of which were fatal.
Host Species
Birds are the primary hosts of the virus, but it can also infect mammals, causing disease in horses and humans (with a steadily increasing number of cases). In rarer instances, infections have also been observed in amphibians and reptiles. However, mammals, including humans, as well as amphibians and reptiles are regarded as dead-end hosts, meaning they do not transmit the virus onward; only birds can sustain the transmission cycle through mosquitoes. Migratory birds may play an important role in spreading the pathogen during their migrations, particularly because some bird species can carry very high levels of the virus with extremely low mortality rates, allowing them to transport it silently even across continents.
Transmission and Vectors
The virus is primarily transmitted via mosquito vectors, but it can also spread, more rarely through bodily fluids, blood transfusion, organ transplantation, and predator–prey interactions. The main vectors are mosquitoes of the genus Culex (family Culicidae), though the virus has been detected in species from ten other genera as well. In Europe, the common house mosquito (Culex pipiens) is considered the most important vector.
Symptoms
In birds, infection manifests mainly as neurological symptoms. Young birds are often affected, and the infection can cause encephalitis and meningitis, leading to movement coordination problems, muscle spasms, neck stiffness, and paralysis. Acute myocarditis and heart muscle damage are also significant, sometimes leading to sudden heart failure and death.
Among mammals, horses are highly susceptible to the virus. Infected horses may develop skin hypersensitivity and fever, and in more severe cases, neurological symptoms and encephalitis.
In humans, approximately 75% of infections are asymptomatic. In less than 20–25% of cases, symptoms resemble influenza, with general fever, headache, muscle weakness, nausea, and loss of appetite. Only about one case of encephalitis or meningitis (neurological disease) occurs per 4,000–5,000 infections.
Treatment and Prevention
There is currently no vaccine available for humans, but a vaccine for horses is available in Hungary.
YELLOW FEVER
Distribution
Yellow fever occurs in West, Central, and East Africa, as well as in South America from Panama to northern Argentina. Its vector, the yellow fever mosquito (Aedes aegypti), once occurred in Europe and was responsible for serious yellow fever outbreaks. After disappearing following World War II, its reappearance and wide spread remain possible, similar to the Asian tiger mosquito (Aedes albopictus), which has re-emerged in Europe in recent years.
Host Species
In forest environments, the virus circulates among non-human primates, while in populated areas it spreads among humans. Every unvaccinated person in an endemic zone is at risk. In recent years, several unvaccinated European and North American tourists have died after visiting affected areas. In certain tropical regions, yellow fever mosquito (Aedes aegypti) is a common and widespread mosquito species, representing a significant infection risk and the potential for large-scale outbreaks.
Transmission and Vectors
Yellow fever is transmitted exclusively through the bite of an infected, virus-carrying mosquito. The most well-known vectors are the yellow fever mosquito (Aedes aegypti) and the Asian tiger mosquito (Aedes albopictus). An infected female mosquito can pass the virus on to the next generation via its eggs. A person without immunity to yellow fever who is bitten by an infected mosquito can themselves become infectious. High levels of the virus are present in the blood from the day before symptoms appear, and typically for the next four days, during which time the person can infect additional blood-feeding mosquitoes.
Symptoms
In African non-human primates, infection is either asymptomatic or causes only mild illness, and it mainly comes to attention when humans become infected. In contrast, the virus is lethal to South American non-human primates, and outbreaks there are often detected because the rainforest falls silent following the death of howler monkeys.
In humans, symptoms appear suddenly, 3–5 days after infection, and can range from mild to fatal. Clinical cases typically present with sudden fever, severe headache, and joint and muscle pain. Jaundice may develop by the third day, and in severe cases spontaneous bleeding, kidney failure, delirium, coma, and death can occur. The case fatality rate in clinical yellow fever can reach up to 80%. Recovery is prolonged and often accompanied by serious complications.
Treatment and Prevention
The YF 17D vaccine provides safe, effective, and low-cost protection against yellow fever and has been used successfully for more than fifty years. Immunity develops ten days after vaccination and lasts for life. The infection can be confirmed by serological testing to detect specific antibodies one week after infection. Once the disease develops, supportive care is the only treatment option. The use of aspirin and other blood-thinning medications is strictly prohibited.
ZIKA FEVER
DISTRIBUTION
The most at-risk areas are the tropical zones and the Mediterranean region, but the virus can appear anywhere, where Aedes mosquitoes can survive. In Brazil, it emerged in the spring of 2015 and spread rapidly throughout the year to several other South and Central American countries. In Europe, Zika virus cases are few and currently imported, however their number is expected to rise due to travel to the most affected regions. Since the virus has been shown to transmit sexually, there is also a non-negligible chance that Zika virus could spread locally.
AFFECTED HOST SPECIES
The full range of vertebrate hosts is not completely known. Most frequently, infections have been reported in humans and non-human primates, but some studies suggest that small mammals (e.g., rodents) can also be infected.
TRANSMISSION AND VECTORS
Zika is primarily transmitted by mosquitoes of the genus Aedes, with the most important vectors being invasive species such as the Asian tiger mosquito (Aedes albopictus). It is not yet known whether other local mosquito species can transmit the virus, but no such cases have been observed in temperate countries. The virus can also be transmitted sexually.
SYMPTOMS
In humans, the disease is usually relatively mild. After a few days of incubation, roughly one-fifth of infected individuals develop general febrile symptoms (fatigue, weakness, nausea), skin rashes, and muscle or joint pain. The illness is generally self-limiting, with symptoms resolving within a few days. Severe symptoms (e.g., neurological complications) are rare. Based on symptoms alone, viral infections cannot be definitively distinguished, so laboratory tests are needed for an accurate diagnosis. Following Zika outbreaks, there was a significant increase in the number of children born with microcephaly, for which the virus was responsible.
TREATMENT AND PREVENTION
Currently, there is no vaccine available against Zika virus. The most reliable protection is to prevent mosquito bites in affected areas. There is no specific treatment for the disease; symptom relief and fever management are possible if needed. Individuals who recover from the infection become virus-free and immune, so fetuses conceived after recovery are not expected to be affected.